How are drugs designed and developed?

Producing a new drug is an expensive and time-consuming process that is subject to extensive regulation.
What is a drug?
Drugs are chemical or biological substances that have some kind of physiological? or biochemical? effect on our bodies.
- They may be single compounds or a mixture of different compounds.
Their effects are intended to be beneficial but can cause harmful side effects in some people.
All drugs interact with specific ‘targets’ in the body, with the aim of modifying their activity and often resulting in a therapeutic? effect. For example, pain relief.
Drugs work either by stimulating or blocking the activity of their targets.
How is a drug developed?
The development of a new therapeutic drug is a complex, lengthy and expensive process.
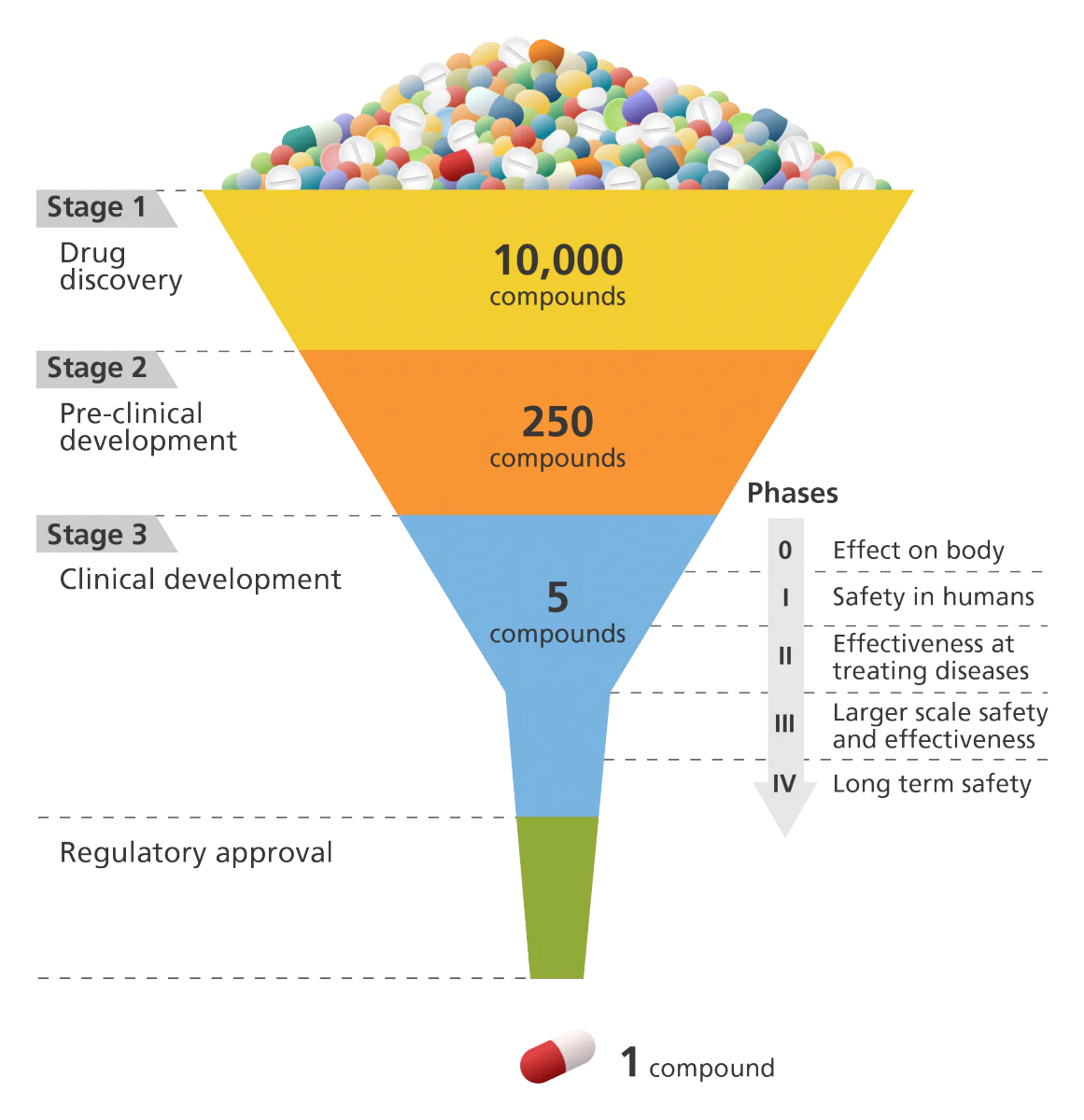
It can take 10-15 years and over £500 million to develop a drug from an initial concept, test its safety and effectiveness in humans and then get it into the hospital market, this includes:
- 2-4 years of pre-clinical development
- 3-6 years of clinical development
- additional time for dealing with the regulatory authorities.
Stage 1: Drug discovery
The first stage of the drug development process is drug discovery.
- In the past, some drugs have been discovered by accident, for example, penicillin.
Today, more systematic approaches are used, such as:
- high-throughput screening: which allows scientists to test thousands of potential targets with thousands of diverse chemical compounds to identify a new drug-target combination.
- rational drug design: which involves designing and synthesising compounds based on the known structure of a specific target molecule.
While high-throughput screening may identify hundreds of potential lead components, many will be eliminated at the first round of testing. During this round compounds are tested in cultured cells or animals to find out how effective they are and whether they have any toxic effects.
Rational drug design develops fewer compounds compared to high-throughput screening. However, these compounds are very specific to the target and use computer-based modelling to achieve this specificity.
Stage 2: Pre-clinical development
Pre-clinical testing is used to determine how best to develop the drug for its intended use.
It aims to establish how drugs are absorbed and distributed in the body, and how they are broken down and removed from the body.
If appropriate, promising drugs may be modified in an attempt to improve their properties in subtle ways in a process called lead optimisation.
The results of pre-clinical testing are also used to determine how to best formulate the drug for its intended clinical use, for example whether it would be most effective as a cream, a pill, an injection or a spray.
The pre-clinical studies aim to whittle hundreds of compounds down to just a few useful candidate drugs.
These few drugs will then be submitted to the appropriate regulatory authorities and, if accepted, the compound can be taken on to clinical development.
Stage 3: Clinical development
- This is divided into Phases 0, I, II, III and IV.
Clinical development, also known as clinical trials, involves testing the drug on human volunteers to provide more information about its safety and effectiveness.
By the end of the clinical development phase, most of the investigational new drugs will have been eliminated on the grounds of safety and effectiveness.
Only one or two compounds will be submitted as a new drug application. In the UK, this is known as a market authorisation application.
After a drug has been approved by the appropriate regulatory bodies, pharmaceutical companies have a short period where only they have the rights to market the drug (exclusivity) and before other companies can market the same drug.
This exclusivity period is used to regain the massive investment required to develop and launch the new drug.
After full approval, drug companies must continue to test their drug and monitor feedback from healthcare professionals to ensure the safety and effectiveness of the drug.
After launching a drug, new side effects or risk factors may be identified that had not been previously recorded. This is Phase IV of clinical development and is part of the continued monitoring of the effectiveness of the drug in their target patients.